 Certainly, here is the rewritten version of the provided text:
Certainly, here is the rewritten version of the provided text:
The diagnosis of breast cancer is difficult to accept. However, the very diagnosis opens a path to hope, determination, and the chance to harness inner strength. Guides like “Breast Cancer: From Discovery to Recovery” are immensely helpful to survivors, particularly those who have had surgery and are in the waiting phase for adjuvant therapy. Using a gentle tone, our aim is to provide survivors with precise, comprehensive, and hopeful guidance regarding the diagnosis, treatment options, and post-treatment care.
Knowing what to expect in every phase—from the diagnosis to the treatment and aftercare—scout a wide range of anxieties tied with unknown aspects. This guide is meant to be by your side, Mason For all of guidance and for all the survivor support, in the attempt to ease the time that struggles the most. We Em power you to accept help of your cancer medical team and the joining and participation in help groups with survivors of the same situation.
Regardless of whether you have just been diagnosed, undergoing treatment, or planning your rehabilitation, we trust this guide is useful both in providing understanding and solace. Let us address the process of diagnosis to enhance understanding.
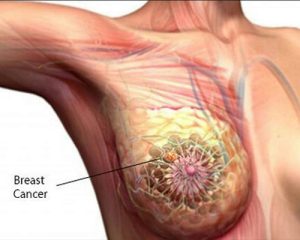
Breast cancer diagnosis might come as a shock, but gaining detailed clarity about the process helps inch anxiety down a notch and equips an individual with detailed insight about their physical well-being. The diagnosis, as one would expect, consists of multiple steps and might include screening, detailed imaging, biopsies, as well as intricate pathological analyses.
The importance of early detection cannot be overstated. A significant portion of breast cancers are discovered during regular check-up tests, which might include:
Should there be any irregularities found in these screenings, it is likely the healthcare professionals will want to carry out further tests.
The biopsy confirms the diagnosis of cancer. It entails extracting a small sample of breast tissue from the suspicious area for microscopic examination. There are several kinds of biopsies:
Following the biopsy, the tissue collection is mailed to the pathology department for slide preparation and microscopy. The pathology report will give the type of breast cancer, the grade (how abnormal the cancer cells look), and other important markers of the cancer.
The pathology report is important because it allows the doctor to plan the treatment. Important parts of the report include:
Your oncologist might ask for further tests to decide how far the disease has spread after the pathology report is evaluated. This evaluation might need:
Your care team needs all this information to fully understand your healthcare needs and prepare an effective treatment strategy.
Feeling a wide range of emotions—from numbing shock and disbelief to restless anxiety and optimistic hope—is to be expected. The following suggestions might help in coping with the emotional distress resulting from your diagnosis:
The diagnosis chapter is challenging for all patients, but know that every page you turn to is a testimony of your bravery and determination to conquer breast cancer.
 After surgery, as you get ready for adjuvant therapy, you should know that effective therapies are available that each aims to lower the risk of it coming back and to assist your body in finishing off any cancer cells that are left. This chapter will discuss the therapies that your care providers may suggest as a result of your diagnosis.
After surgery, as you get ready for adjuvant therapy, you should know that effective therapies are available that each aims to lower the risk of it coming back and to assist your body in finishing off any cancer cells that are left. This chapter will discuss the therapies that your care providers may suggest as a result of your diagnosis.
Adjuvant therapy refers to any treatment provided after the primary surgery aimed at lowering the risk of the cancer coming back. Based on the type, size, and stage of your cancer, your doctor may suggest one or more of the following treatments:
Your oncology team will assess your situation, incorporating your cancer stage, tumour biology, general health, and many other factors to create a tailored treatment plan.
For a large number of patients, chemotherapy is the primary pillar for adjuvant treatment. The medications used in chemotherapy medications also destroy other rapidly growing cells in the body. While this treatment lowers the chances of a disease relapse, it may also cause several side effects including exhaustion, vomiting, hair shedding, and greater chances of contracting infections.
Make sure to touch base with your oncologist regarding chemotherapy—what you should expect and how best to manage the side effects. Many find that exercise, proper nutrition and even gentle physical activity can lessen the impact of side effects as well as mindfulness exercises.
Post-breast conserving surgery or lumpectomy, radiation therapy is ordinarily ordered. Its purpose is to mop up any lingering microscopic cancer cells in the breast or chest wall. With modern breast cancer treatment, the radiation therapy procedures have become very focused, which aids in protecting healthy adjacent tissues.
The possible side effects of radiation include skin irritation, tiredness, and alterations in breast tissue. It is best to shield your skin and heed your body’s needs during the treatment. Your radiation oncologist will give you radiation therapy protocols on how to deal with the side effects.
In cases of hormone receptor-positive breast cancer, hormone therapy becomes integral to the treatment. Drugs such as tamoxifen and aromatase inhibitors block estrogen’s effects or reduce its levels in the body, halting the progression of hormone-sensitive breast cancer.
Hormone therapy is generally prescribed for several years. Despite being largely effective, it may cause some side short-term effects such as hot flashes, joint pain, and mood changes. Your oncologist will be able to effectively manage your hot flashes and other side effects to maintain your quality of life via regular follow-up visits.
Targeted therapy is a valuable treatment option for cancer that overexpresses the HER2 protein. The use of drugs such as trastuzumab, which specifically target HER2-positive cells, limits the damage to normal tissues. The use of this therapy, in conjunction with chemotherapy, has markedly improved the prognosis of a large portion of the patients.
Targeted therapy is constructed based on the molecular features of your tumor and might be used alongside hormonal and chemotherapy treatments for the best possible outcome.
What immunotherapy is trying to achieve is a new and promising direction in the treatment of breast cancer. Specifically, it will attempt to use the body’s immune system to identify and attack cancer cells. If you want to learn more about treatment options and clinical trials, make sure to bring this up to your oncology team. Clinical trials are currently being conducted, and it is a great option worth exploring.
Keeping updated on newly developed breast cancer treatments might allow you to further improve your care and make use of the general survivor resources offered to the public.
Selecting the appropriate adjuvant treatment involves a careful decision-making process that should involve your oncologist. You should take into account:
Make sure to gather enough information through questions and, if necessary, second opinions. Each option in this breast-cancer recovery guide is effective for reducing the likelihood of it coming back and should be regarded as complementary.
Before starting the adjuvant therapy, please get in touch with your oncology team for a consultation to receive effective guidance for your treatment.
After the initial treatment, temporary therapies are equally as critical as dealing with the support after treatments. In the recovery process, there is the need for recuperation emotionally and socially, alongside physical healing. Here, we look at the different methods to assist you as you progress in life.
The challenges brought about by breast cancer affect one beyond the struggles of the body. It is typical for survivors to go through episodes of anxiety, depression, and even a feeling of being cut off from the world, especially when dealing with the aftermath of the treatment. To assist your emotional recovery, look into the following:
Keep in mind that seeking assistance demonstrates courage. Your oncology team can guide you to integrated psychosocial support services if PST feels too much to handle.
The aftermath of breast cancer treatment can at times feel quite isolating. Mental wellness can be aided by socializing with individuals who have a similar background. You can check the following out:
These groups are tremendously helpful in assuring you that there are others to support you as you recover from breast cancer.
As you continue, making healthy lifestyle choices daily can be immensely beneficial to your recovery as a whole. They include the following:
Lifestyle management improves not only one’s physical health but also one’s mental and emotional fortitude.
Survivors of cancer treatment report that integrative therapies work well along with standard treatments. These therapies and treatments include:
Such treatments, although helpful, must be evaluated by a medical professional in order to check if they do not hinder other treatments.
The financial impact of cancer treatment is often profound. The following practical support services may help alleviate these concerns:
Issues like these require people to address and resolve them, and we strongly encourage you to make use of all the help and support that is available. Your physical and mental health is of utmost importance and there are several helpful resources that are designed to enable your smooth transition into life after treatment.
A: The diagnosis phase usually starts with a mammogram or an ultrasound. If cancer-cell presence is suspected, a biopsy is done for confirmation. For your specific case, further imaging like MRI or CT scan along with PET scan may be done.
A: Treatment is tailored to your unique situation depending on the cancer stage and hormone receptor status, as well as your general health and treatment preferences. You should discuss the details of your treatment plan with your oncology team so that you can weigh all options and make a wise choice.
A: You may experience side effects such as tiredness, nausea, and hair loss as well as a greater risk of infection. Your oncology team will ensure proper supportive care and medications to control these side effects. Your team will also ensure that the treatment is customised to lessen distress and ensure your well-being.
A: After the treatment is complete, patients report a change in energy level and cognitive as well as emotional function. It is critical to have continuous follow-ups with your healthcare system team where, not only will they check and treat the later side effects, but, if need be, they will modify their plan of recovery.
A: Emotional support matters a lot. Speaking with a counselor, practising mindfulness, and engaging in yoga or meditation can help alleviate stress. Furthermore, participating in a support group can provide you with valuable connections and a sense of community.
A: Having an appropriate diet, engaging in some form of physical exercise, and practising some kind of stress management can make a big difference in recuperation. Giving up smoking and moderating the intake of alcoholic beverages may be suggested. It is important that such changes are discussed with the treatment providers so that the overall plan is facilitated in an effective manner.
A: You can find support and resources both in your local area and online. They can be obtained by contacting cancer support groups, using well-known cancer websites, and asking for guidance from your medical team. Do not forget that there is help available for you; look into support networks for continuous assistance and friendship.
Transforming from the initial shock of the breast cancer diagnosis to a healing phase offers its own sets of trials and milestones. Being armed with the knowledge of the nuances of diagnosis, the spectrum of treatment choices, and the resolute post-treatment care can greatly support your journey.
During this time, engaging with your oncology team and utilizing the available survivor assistance resources is crucial. You may contact survivors who have undergone breast cancer to offer you support, join their support groups, or even use the communities made by them for survivors. Each and every one of these services is made to support your journey in fighting breast cancer.
You should always stay informed and connected, as well as ask for assistance whenever you need it. Overcoming these challenges inspires not just yourself but a multitude of people who are battling cancer, and your determination and strength is admirable.
Each and every step you take moves you closer to a life abundant with well-being, renewed hope, and endless possibilities. To get more assistance, keep visiting your oncologists and delve into the survivor services that are offered to you both virtually as well as through the community.